Maternal mortality is a pressing concern that continues to spark debate and drive research within the realm of U.S. maternal health. Alarmingly, the United States reports some of the highest maternal mortality rates among high-income nations, highlighting substantial gaps in care and outcomes for women during and after pregnancy. Recent studies indicate that a significant proportion of pregnancy-related deaths are preventable, yet persistent disparities in maternal mortality affect various racial and ethnic groups throughout the country. As these disparities continue to grow, it becomes increasingly critical to address the systemic issues surrounding postpartum care and equitable access to healthcare. Understanding the complex factors contributing to high maternal mortality rates can help us develop effective solutions and ultimately foster healthier mothers and babies across America.
The issue of maternal deaths during childbirth represents a significant dimension of public health that severely affects women’s lives and wellbeing. Often described as pregnancy-related deaths, the statistics reveal concerning trends that demand immediate action. The disparities in mortality rates experienced by different communities underscore the urgent need for targeted interventions in U.S. maternity care. As we delve into the realities of maternal health, it is vital to consider not only prenatal appointments but also the quality of postpartum support available to mothers. Addressing these elements can pave the way for improved outcomes, diminishing the shocking figures related to maternal mortality and pregnancy-related fatalities.
Understanding High Maternal Mortality Rates in the U.S.
The United States stands out for having the highest maternal mortality rates among high-income nations, prompting urgent discussions around the underlying causes. A staggering 80 percent of these pregnancy-related deaths are deemed preventable, yet the upward trend in statistics reveals deep-rooted flaws in the healthcare system. Several potential factors contribute to this alarming reality, including a fragmented healthcare network, inadequate access to care, and socio-economic disparities affecting vulnerable populations, particularly Black, Indigenous, and other marginalized groups.
Examining the data from the Centers for Disease Control and Prevention, it becomes evident that racial disparities persist in maternal health. For instance, American Indian and Alaska Native women face a mortality rate nearly four times higher than that of white women, underscoring the inequities that plague the system. High maternal mortality rates are not only a reflection of healthcare access but also point to systemic biases and chronic health conditions that disproportionately affect certain groups. Addressing these disparities requires comprehensive policy reform and targeted interventions.
The Role of Postpartum Care in Reducing Maternal Mortality
Postpartum care plays an essential role in the continuum of maternal health, especially given that nearly one-third of pregnancy-related deaths occur after the initial postpartum period. A traditional view often limits postpartum care to just a six-week check-up, leaving new mothers without the necessary support as they navigate the challenging recovery period. Recognizing that the postpartum phase extends far beyond these arbitrary time frames is critical to lowering maternal mortality rates. Continual healthcare access during this phase can significantly impact long-term maternal health outcomes.
Moreover, the COVID-19 pandemic has highlighted just how vital it is to provide comprehensive care during the postpartum period. With rising incidents of late maternal deaths, there is an urgent need for healthcare systems to adapt to the challenges encountered by new mothers within this timeframe. Innovations in postpartum care models must incorporate mental health resources and chronic disease management to better address the complexities of maternal health. By investing in sustained support systems for mothers, we can decrease the likelihood of preventable deaths and improve overall maternal health.
Racial Disparities in Maternal Health Outcomes
Racial disparities in maternal mortality statistics reveal a sobering reality about health equity in the United States. The mortality rates for American Indian, Alaska Native, and Black women emphasize a crisis that transcends individual health and speaks to a broader systemic neglect. The fact that despite years of research and targeted interventions, significant gaps persist underlines the complexity of addressing these disparities. Factors like implicit bias within healthcare providers, socio-economic barriers, and insufficient access to quality prenatal care converge to exacerbate risks for women of color during pregnancy and childbirth.
Addressing these disparities requires more than just awareness; it demands action from healthcare systems, policymakers, and community organizations. Initiatives need to focus on creating equitable access to care and tailored support that recognizes the unique challenges faced by different populations. Additionally, fostering community-based programs can empower women, ensuring they are informed and engaged throughout their pregnancy and early postpartum period. Only through commitment to equity-driven solutions can we hope to dismantle the systemic barriers contributing to racial disparities in maternal mortality.
Policy Changes Needed to Combat Maternal Mortality
Effective policy changes are paramount in the fight against rising maternal mortality rates in the United States. The current landscape reveals a patchwork of healthcare access that varies wildly between states, leading to significant differences in maternal health outcomes. States that prioritize maternal health have demonstrated better results, suggesting that national standards are necessary to ensure all women receive equitable care. Advocacy for comprehensive health policies that focus on maternal well-being and access to prenatal and postpartum care is critical to reversing these trends.
Furthermore, as funding for maternal health programs continues to dwindle, there is an urgent need to rally support for public health infrastructure. Sustained investment in maternal health research, education, and community health programs can effectively reduce pregnancy-related deaths. Policymakers must prioritize maternal health within the broader context of public health; an integrated approach that addresses health inequities will be essential in ultimately enhancing outcomes for mothers across the nation.
Innovations in Maternal Health Care Delivery
Innovative approaches to maternal healthcare can significantly impact the reduction of high maternal mortality rates in the U.S. Telehealth services, for example, have emerged as a critical resource, especially during the COVID-19 pandemic, by bridging gaps in access to timely care. Such platforms allow healthcare providers to monitor mothers’ conditions, offer medical advice, and conduct follow-ups without requiring in-person visits, which can often be a barrier due to transportation or other logistical issues. By expanding these services, healthcare providers can improve prenatal and postpartum care for many underserved populations.
Moreover, integrating mental health services into maternal care models is another innovative solution that addresses a neglected aspect of postpartum health. Mental health challenges, such as anxiety and depression, are prevalent among new mothers and can significantly affect their well-being. By ensuring that maternal healthcare systems include robust mental health screening and support, we can create a more comprehensive care model that encourages mothers to seek the help they need. These innovations, coupled with community engagement and targeted outreach, hold promise in ultimately reducing maternal mortality and improving health outcomes across diverse demographics.
The Impact of Chronic Conditions on Maternal Health
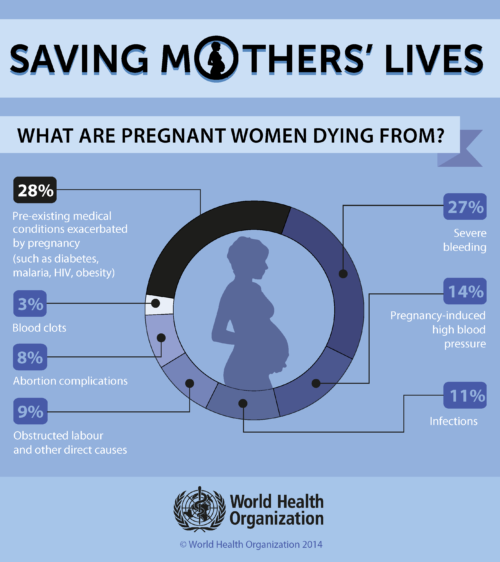
Chronic health conditions among women of reproductive age pose a significant challenge to maternal health, contributing to rising rates of pregnancy-related deaths. Issues such as hypertension, diabetes, and obesity have all been linked to higher risks during pregnancy and childbirth. The increased prevalence of chronic conditions, particularly in younger populations, indicates that many potential mothers are entering pregnancy with pre-existing health issues that complicate their care. As cardiovascular disease has become the leading cause of maternal death, addressing these underlying chronic conditions is paramount.
To effectively combat the rise in maternal mortality, healthcare systems must prioritize preventive measures and management strategies for chronic diseases among reproductive-age women. This includes regular health screenings, lifestyle education, and comprehensive management plans that span preconception through postpartum care. By proactively addressing these health issues, we can significantly improve health outcomes for expectant mothers and reduce the impact of chronic conditions on maternal mortality.
The Importance of Data Collection in Maternal Health
One of the key hurdles in addressing maternal mortality rates is the challenge of data collection and analysis. Historically, the United States lacked a standardized system for tracking maternal deaths, which hindered the ability to identify trends and target interventions effectively. Since the implementation of the pregnancy checkbox on death certificates, researchers have gained invaluable insights into maternal mortality trends and causes. This improved data collection process is crucial, as it provides a clearer picture of the maternal health landscape and informs policy decisions.
However, even with enhanced data collection, disparities remain in documenting and understanding maternal mortality in diverse populations. It’s imperative that future data initiatives focus on capturing more comprehensive demographic information to better elucidate the factors contributing to deaths. Understanding the nuances of various racial, ethnic, and socio-economic contexts will enable more effective targeted policies and programs aimed at reducing maternal mortality rates across the board.
Future Directions for Maternal Health Advocacy
Maternal health advocacy is at a critical juncture, with rising maternal mortality rates underscoring the need for coordinated action. It is essential for advocates to mobilize community support and engage with policymakers to raise awareness of this urgent issue. Emphasizing the preventable nature of most pregnancy-related deaths can galvanize efforts to institute necessary reforms and allocate resources towards maternal health initiatives. Grassroots campaigns, alongside professional organizations, can drive change by pushing for policies that ensure quality care throughout the pregnancy and postpartum periods.
Furthermore, collaborations between healthcare professionals, policymakers, and community organizations can foster a more holistic approach to maternal health. By sharing insights, resources, and best practices, stakeholders can create comprehensive plans that address the multifaceted factors influencing maternal mortality. Through advocacy that emphasizes equitable access to care and community engagement, it is possible to cultivate a healthcare environment where every woman receives the support she needs during and after pregnancy.
Addressing Social Determinants of Health in Maternal Care
Social determinants of health—including socioeconomic status, education, and access to healthcare—play a pivotal role in maternal health outcomes. Acknowledging that these determinants can exacerbate the risks associated with pregnancy is crucial for developing effective strategies to combat maternal mortality. For many women, factors such as lack of transportation, unstable housing, or insufficient healthcare coverage can directly impact their ability to access essential maternal care services. As a result, addressing these broader social issues is vital in the push to lower maternal mortality rates.
Efforts to improve maternal health should increasingly incorporate initiatives that support social determinants. For example, providing transportation services for medical appointments or establishing community health programs that address housing stability can alleviate some of the barriers to accessing care. By creating a more supportive environment for expecting and new mothers, we can mitigate the risks associated with maternal health disparities and improve health outcomes for all women, regardless of their socio-economic situation.
Frequently Asked Questions
What are the main causes of high maternal mortality rates in the U.S.?
High maternal mortality rates in the U.S. stem from various factors, including an inequitable healthcare system, lack of access to comprehensive prenatal care, and systemic biases affecting minority populations. According to recent studies, cardiovascular diseases are now the leading cause of pregnancy-related deaths, accounting for over 20% of such fatalities.
How do disparities in maternal mortality affect different racial and ethnic groups?
Disparities in maternal mortality rates highlight significant differences between racial and ethnic groups in the U.S. For instance, American Indian and Alaska Native women face a mortality rate nearly four times higher than white women. These disparities suggest that systemic inequities and biased healthcare practices continue to impact maternal health significantly.
What role does postpartum care play in preventing pregnancy-related deaths?
Postpartum care is crucial in reducing pregnancy-related deaths, particularly since many deaths occur between 42 days to one year after delivery. Recognizing that postpartum recovery is not limited to the first six weeks, improved access to extended postpartum care can address health issues that arise during this vital period.
Why is the U.S. maternal health system considered to have a high maternal mortality rate compared to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries due to several factors, such as a fragmented healthcare system, maternity care deserts, and increasing rates of chronic health issues among reproductive-age individuals. These systemic shortcomings have resulted in more preventable pregnancy-related deaths.
What measures can be taken to improve U.S. maternal health outcomes?
Improving U.S. maternal health outcomes requires investing in public health infrastructure, enhancing prenatal and postpartum care, and addressing state-specific disparities. Policy reforms aimed at standardizing care and increasing access to quality healthcare are essential in tackling the rising rates of pregnancy-related deaths.
How does the COVID-19 pandemic influence maternal mortality rates?
The COVID-19 pandemic has had a significant impact on maternal mortality rates, with a noticeable rise in deaths starting in 2021. The pandemic’s effects on healthcare access, combined with the increased prevalence of chronic conditions, have likely contributed to this troubling trend in maternal health.
What is considered a late maternal death, and why is it significant?
A late maternal death refers to fatalities occurring between 42 days and one year post-pregnancy. This classification is significant because it underscores the need for continuous healthcare support beyond the traditionally recognized postpartum period, highlighting the importance of sustained maternal healthcare.
What can be done to address the preventable aspects of pregnancy-related deaths?
To address preventable pregnancy-related deaths, there needs to be a focus on enhancing access to quality prenatal and postpartum care, implementing effective education programs for healthcare providers, and addressing social determinants of health that disproportionately affect at-risk populations.
| Key Point | Details |
|---|---|
| U.S. Maternal Mortality Rate | The U.S. leads high-income countries in maternal mortality with significant increases observed from 2018 to 2022. |
| Preventability | Over 80% of pregnancy-related deaths in the U.S. are preventable, highlighting flaws in the healthcare system. |
| Racial Disparities | American Indian and Alaska Native women face the highest mortality rates, nearly four times that of white women. |
| Impact of COVID-19 | The pandemic likely contributed to a spike in maternal mortality rates in 2021. |
| Chronic Conditions | There is a growing incidence of chronic conditions like cardiovascular disease among pregnant individuals. |
| Postpartum Mortality | ‘Late maternal deaths’ occurring up to one year post-birth accounted for nearly a third of total deaths. |
| Policy Recommendations | Investing in public health infrastructure and improving healthcare systems for better pregnancy and postpartum care is essential. |
Summary
Maternal mortality remains a critical issue in the United States, marked by rising rates and significant disparities among different racial groups. Addressing this crisis requires a comprehensive approach to improving prenatal and postpartum care while tackling systemic inequities in the healthcare system. As we see that over 80% of these deaths are preventable, it is imperative to enhance policy initiatives and health infrastructure to ensure safe pregnancies for all women.