CRISPR Gene Editing: Ethics and Innovations in Healthcare
CRISPR gene editing has recently emerged as a groundbreaking solution in the field of medical innovation, particularly in the quest to find a cure for diseases like sickle cell anemia. This powerful technology allows scientists to modify genetic material with unprecedented precision, offering new hope for patients suffering from genetic disorders. However, the application of CRISPR raises vital gene editing ethics questions that society must confront. As researchers explore the potential for health equity, the implications of editing the human genome become complex and multifaceted. With great power comes great responsibility, leading us to grapple with who decides which traits are enhanced and which conditions are treated.
Gene editing technologies, especially CRISPR, have revolutionized how we approach genetic diseases, showcasing a remarkable leap in biomedical science. Various terms surround this transformative method, including genetic alteration and targeted gene therapy, reflecting its intricate role in contemporary medicine. As we delve into discussions about the potential for curing debilitating conditions like sickle cell disease, considerations of medical ethics and societal implications loom large. Furthermore, the intersection of these innovations with concepts of health equity raises pressing questions about access and fairness in healthcare. The ongoing dialogue about these advancements emphasizes the necessity of addressing ethical concerns while harnessing the benefits of this powerful technology.
Understanding CRISPR Technology and Its Implications
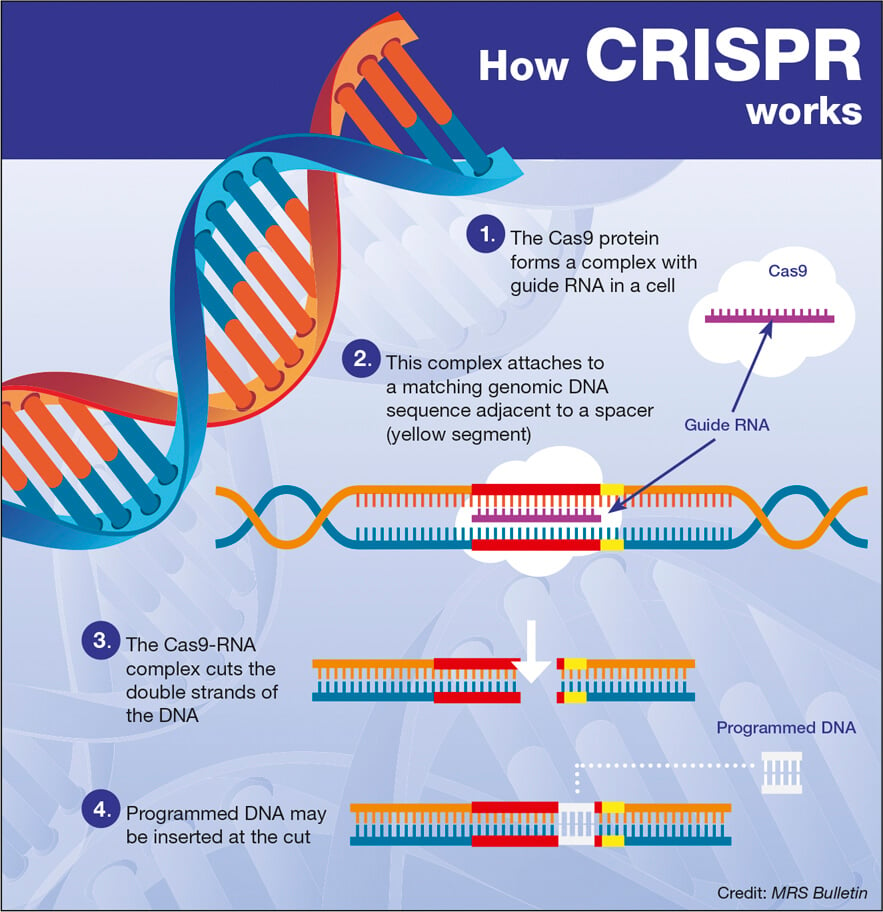
CRISPR technology represents a groundbreaking advancement in genetic engineering, enabling scientists to make precise alterations to DNA sequences. This technique utilizes a programmable RNA and a Cas9 protein, which acts as molecular scissors to cut DNA at specific sites. The ability to remove or replace defective genes paves the way for potential cures for genetic disorders such as sickle cell anemia. However, while CRISPR holds tremendous promise for medical innovation, its implications are vast and require careful consideration of ethical dimensions. As we explore the potential of CRISPR in health settings, we must also confront the nuanced questions of morality and fairness in access to these treatments.
The application of CRISPR technology extends beyond disease prevention to considerations of enhancement, raising ethical debates about the very essence of what it means to be human. In the aforementioned discussion led by Neal Baer, one poignant question raised was whether gene editing should be employed for conditions seen as life-compatible, like Down syndrome. This thought-provoking inquiry challenges our society to consider deeply the implications of genetic modifications and the potential for societal division based on these advancements. As we navigate this terrain, balancing progress with principled discussions about human variation and health equity will be crucial.
Ethics of Gene Editing and the Responsibility of Innovation
The ethics of gene editing cannot be overstated, especially as innovations like CRISPR gene editing become more prevalent in medicine. The talk by Neal Baer underscored critical questions about our responsibility towards those who could be affected by gene modifications. With remarkable innovations come great responsibilities; we must ponder who gets to decide on which diseases or traits can be altered. The discussions surrounding the ethical implications of gene editing compel us to confront our biases and societal narratives about health and normalcy, especially for conditions traditionally seen as disabilities.
Moreover, the concept of health equity plays a pivotal role in the ethical landscape of gene editing. As Baer highlighted, the prohibitive costs associated with treatments, such as the proposed $2.2 million for curing sickle cell, raise critical equity issues. These considerations force us to examine whether such technologies will be accessible to all or merely to those with substantial resources. Thus, initiating dialogue about these ethical dilemmas is essential to ensure that we do not create a divide between the haves and have-nots in the realm of medical innovations.
The Promise of a Sickle Cell Cure: Consequences and Considerations
Sickle cell anemia, a hereditary condition causing severe pain, strokes, and significant health issues, stands as a key focus in discussions about the promise of CRISPR gene editing. The potential for a cure through gene manipulation offers hope to many families suffering from this devastating disorder. Baer emphasized that beyond the excitement surrounding this medical breakthrough, there are significant considerations to account for, including the emotional weight of altering human genetics. How do we measure the value of a life when subjected to the lens of genetic correction? This question becomes particularly poignant when considering the diverse perspectives on disability within society.
The discussions surrounding the use of CRISPR for sickle cell also prompt broader concerns about medical ethics and social implications. As highlighted by Baer and Brendel during the talk, intentional decision-making in health care must prioritize not only medical outcomes but also societal impacts. For instance, organizations and policymakers must consider who has access to these advancements and how they contribute to overarching narratives about health equity. Without mindful oversight, the advancements in treating conditions like sickle cell could reinforce existing disparities in healthcare access and health outcomes.
Health Equity in the Age of Gene Editing
The integration of CRISPR gene editing technology into medical treatments brings forth essential dialogues regarding health equity. As new therapies emerge that can alleviate or cure genetic diseases, the question of who can access these treatments becomes paramount. Neal Baer’s insights highlight that while CRISPR may offer cures for ailments such as sickle cell anemia, the financial implications of such treatments could exacerbate healthcare disparities. Thus, there’s a pressing need for frameworks that ensure equitable access to gene editing innovations, preventing the creation of a two-tier healthcare system where only the affluent can afford life-saving interventions.
Health equity should be intertwined with discussions about medical innovation, such as CRISPR. Policymakers and healthcare providers must advocate for inclusive practices that prioritize all individuals, especially marginalized communities disproportionately affected by genetic disorders. Tackling these issues involves committed dialogue about funding allocations, societal impacts, and ethical norms. As we advance into an era where gene editing can radically change lives, the focus on equitable healthcare access must remain steadfast to ensure that no community is left behind.
The Risks of Unregulated Gene Editing
As the field of CRISPR gene editing evolves, so do concerns over the potential risks associated with unregulated practices. Baer’s cautionary remarks regarding oversight resonate deeply, particularly given the implications of rogue scientific practices that may emerge globally. The ability to edit genes irresponsibly could lead to unforeseen consequences, not just for individuals but for societal well-being at large. Ensuring robust regulatory frameworks will be crucial in navigating the complex landscape of gene editing technology while safeguarding humanity against potential misuse.
Moreover, the historical lessons about medical experimentation and human rights compel us to demand stringent regulations around gene editing technologies. The prospect of germline editing—altering genes in embryos—carries an inherent risk of unknown long-term effects, both genetically and ethically. Baer’s references to practices in countries with lax regulations illustrate how important it is for global standards to be established and upheld. The moral imperative to protect future generations from potentially harmful alterations is central to responsible innovation.
Innovative Treatments and Genetic Modification
The advent of CRISPR has created a compelling opportunity for innovative treatments in genetics. While the technology promises to address various ailments through genetic modification, it also invites scrutiny concerning the breadth of its applications. For instance, how do we determine what constitutes a necessary modification versus what may be classified as ‘enhancement’? This question puts a spotlight on the ethical dilemmas innate to gene editing, forcing medical professionals and ethicists alike to grapple with definitions of disease and the pressures of societal norms.
As medical innovations continue to rise, careful considerations must accompany new technologies. Stakeholders in health care, from researchers to clinicians, need to engage in ongoing conversations about the societal impacts of these advancements. As noted during the discussion led by Baer, it is essential that innovation in gene editing aligns with moral and ethical standards, ensuring that the drive for technological advancement is matched by a commitment to responsible, equitable, and conscientious application.
Parental Choices in Genetic Engineering
One of the most profound aspects of CRISPR technology involves the agency parents might wield in deciding the genetic attributes of their offspring. Baer raised thought-provoking inquiries regarding the parental responsibility in selecting traits or eliminating certain conditions from their children’s genetic makeup. This contemplation aligns with broader ethical discussions about ‘playing God’ and the implications of creating preference-based genetic alterations. The potential to engineer desired traits opens a Pandora’s Box of moral questions that society must address seriously.
For future generations, the ability to shape genetic characteristics may redefine the relationship between parents and children. As highlighted by Baer, individuals from different backgrounds may view these possibilities through various lenses. Therefore, ongoing discourse about the ethical limits of parental choice must accompany the rapid advancements in gene editing capabilities, ensuring that society grapples with the potential repercussions of genetically modified offspring.
Monitoring Genetic Engineering Research Globally
The call for rigorous oversight of gene editing technologies echoes throughout discussions on ethical medical practices, particularly concerning global research efforts. With countries such as China and Russia potentially operating outside the stringent regulatory measures preferred in places like the United States, Baer’s concerns highlight an urgent need for unified international standards in genetic research. As gene editing technology advances, having a robust monitoring system in place is paramount to ensuring responsible practice, reducing unethical experimentation, and protecting vulnerable populations.
Furthermore, fostering international collaboration on gene editing practices could help establish best practices and share models for ethical oversight. As various countries explore the potential benefits of CRISPR and other gene-editing technologies, they simultaneously expose themselves to the potential of misuse. Thus, establishing frameworks that invite global dialogue and accountability about ethical practices in genetic engineering is essential to shape a favorable trajectory for medical innovation.
Future Directions in Gene Editing and Health Outcomes
Looking to the future, the intersection of CRISPR technology and health outcomes is ripe for exploration and enhancement. As innovative methods of gene editing emerge, so too does the potential to transform how we approach currently incurable diseases. Shaping policies that foster innovation must involve an ethical commitment to ensuring that advancements in gene editing improve health outcomes for all, particularly individuals currently facing significant barriers to care. Each step forward should ideally provide more equitable access to groundbreaking treatments.
Moreover, the impact of gene editing on public health cannot be understated. As we tread carefully into this rapidly advancing field, engaging diverse communities in conversations about gene editing and its implications will be essential. By prioritizing ethical standards and health equity from the outset, we have the opportunity to not only innovate in medicine but also to establish a comprehensive framework that ensures health improvements are sustained and shared broadly across society.
Frequently Asked Questions
What is CRISPR gene editing and how does it work?
CRISPR gene editing is a revolutionary technology that allows scientists to modify an organism’s DNA with precision. By utilizing a naturally occurring system in bacteria, CRISPR uses a guide RNA to locate a specific sequence in the DNA, and the CRISPR-associated protein (often Cas9) cuts the DNA at that site. This enables the removal or addition of specific genes, paving the way for potential cures for genetic diseases such as sickle cell anemia.
What are the ethical concerns surrounding CRISPR gene editing?
The ethical concerns surrounding CRISPR gene editing include questions about the safety and long-term effects of altering genes, especially in germline editing where changes can be inherited by future generations. Debates also focus on the potential for creating ‘designer babies’ and the social implications, such as health equity and access to expensive treatments. Experts caution that innovations must be accompanied by ethical considerations to prevent exacerbating inequalities in healthcare.
How does CRISPR gene editing promise a cure for sickle cell anemia?
CRISPR gene editing offers a promising cure for sickle cell anemia by enabling precise modifications to the genes responsible for the disease. By editing the somatic cells of patients, scientists can correct the genetic mutations that cause sickle-shaped red blood cells. This leads to improved health outcomes for patients, potentially alleviating the severe symptoms associated with the disease.
What role does health equity play in CRISPR gene editing advancements?
Health equity is a critical concern in the advancements of CRISPR gene editing, particularly regarding access to these groundbreaking technologies. As treatments like those for sickle cell anemia can be prohibitively expensive, discussions around who can afford genetic therapies and how these innovations affect underserved communities are essential. Ensuring equitable access is vital to prevent further disparities in health outcomes.
What implications does CRISPR gene editing have for medical innovation?
CRISPR gene editing signifies a major leap in medical innovation, with the potential to transform the treatment of various genetic disorders. However, it’s essential to balance this innovation with ethical considerations to navigate the promise and peril of altering human genetics. Ongoing discussions about its implications aim to ensure that breakthroughs benefit all of society and do not deepen existing inequalities.
| Key Point | Details |
|---|---|
| Ethical Questions | Is it right to change human differences? Discussed by Neal Baer in the context of CRISPR. |
| CRISPR Capabilities | CRISPR allows editing of somatic and germline genes, potentially curing genetic diseases like sickle cell. |
| Cost and Access | The sickle cell ‘cure’ costs around $2.2 million, raising issues of who can afford treatment. |
| Health Equity | Innovation may increase disparity in health access, necessitating ethical considerations. |
| Parental Rights | Debate exists over whether parents should decide on genetic attributes for their children. |
| Oversight Issues | Concerns about monitoring and regulation of gene editing, especially in countries with less oversight. |
| Possible Unintended Consequences | Editing genes may lead to unforeseen effects, as genes have complex interactions. |
Summary
CRISPR gene editing represents a groundbreaking advancement in the field of genetics, allowing scientists to modify genes responsible for various diseases. While the potential benefits of CRISPR are immense, such as curing conditions like sickle cell anemia, it raises significant ethical questions regarding human intervention in natural genetic variation. As we stand at the intersection of innovation and ethics, the discourse surrounding CRISPR emphasizes the need for careful consideration of health equity, oversight, and the implications of modifying human genetics.